Are you curious about calculus teeth and eager to broaden your knowledge on this topic? In this ultimate guide, we will delve into the fascinating world of calculus teeth, covering everything from their function to their importance in the dental field.
Recent studies have shown that understanding calculus teeth is crucial in maintaining good oral health, as they can lead to more serious issues if not properly addressed. By the end of this guide, you will have a comprehensive understanding of calculus teeth and how to effectively manage them.

The Importance of Calculus Teeth in Dental Health
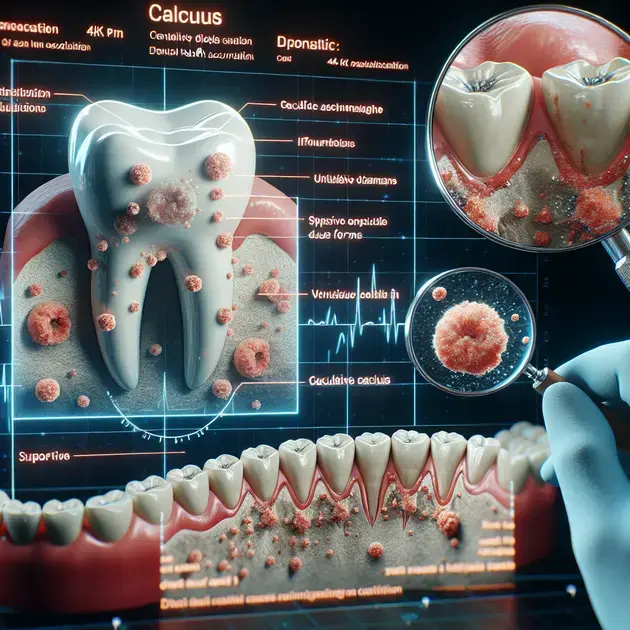
Calculus teeth, also known as tartar, can have a significant impact on dental health. When plaque, a sticky film of bacteria, builds up on teeth and hardens into calculus, it can lead to various oral health issues such as gum disease, cavities, and bad breath. Therefore, it is crucial to understand the importance of managing calculus teeth for overall dental well-being.
One effective way to address calculus teeth is through regular dental cleanings. Dentists use special tools to safely remove calculus buildup from teeth, helping to prevent further oral health complications. These cleanings typically involve scaling to remove calculus from the tooth surfaces and root planing to smooth the tooth roots and prevent future buildup.
Additionally, maintaining good oral hygiene practices at home can help prevent calculus buildup. Brushing your teeth twice a day with a fluoride toothpaste, flossing daily, and using an antiseptic mouthwash can all contribute to reducing plaque and calculus formation.
For a comprehensive understanding of the importance of calculus teeth in dental health, websites like WebMD and the American Dental Association offer valuable information and resources on oral care. These resources can provide insights into the risks associated with calculus buildup and the importance of preventive measures.
By prioritizing the management of calculus teeth, individuals can maintain optimal dental health and prevent more serious oral conditions in the long run.
Understanding the Function of Calculus Teeth
Calculus teeth serve as a breeding ground for harmful bacteria that can contribute to dental problems if not properly managed. Understanding the function of calculus teeth involves recognizing their role in promoting plaque formation and increasing the risk of gum disease.
One of the key functions of calculus teeth is to provide a rough surface for bacteria to adhere to, making it easier for plaque to accumulate and harden. This process can lead to inflammation of the gums, known as gingivitis, and, if left untreated, can progress to more severe gum disease.
Furthermore, calculus teeth can act as a barrier that protects bacteria, making it harder to remove through regular brushing alone. This protection can exacerbate oral health issues and necessitate professional intervention to effectively remove the calculus buildup.
Online platforms such as Colgate and Healthline offer detailed insights into the function of calculus teeth and the implications for oral health. These resources can help individuals understand the link between calculus buildup and dental problems, highlighting the importance of timely intervention.
By gaining a deeper understanding of the function of calculus teeth, individuals can take proactive steps to manage their oral health and minimize the risks associated with calculus accumulation.
Effective Management Strategies for Calculus Teeth
Effective management of calculus teeth is essential for maintaining optimal dental health and preventing oral complications. Implementing strategies to address calculus buildup can help individuals reduce the risk of gum disease, cavities, and other dental issues.
One management strategy for calculus teeth is to schedule regular dental check-ups and cleanings. Dentists can identify and remove calculus deposits that have accumulated on the teeth, preventing further damage to oral tissues and reducing the risk of infections.
Another effective strategy is to adopt proper oral hygiene habits, including brushing, flossing, and using mouthwash. Brushing with a fluoride toothpaste can help remove plaque before it hardens into calculus, while flossing can reach areas between teeth that are prone to buildup.
In addition, incorporating dietary changes such as reducing sugary and starchy foods can contribute to better oral health and minimize calculus formation. Consuming a balanced diet rich in vitamins and minerals can support overall dental well-being.
Websites like Crest and Delta Dental offer valuable tips and resources on effective management strategies for calculus teeth. These platforms provide guidance on preventive measures, treatment options, and lifestyle changes that can help individuals take control of their oral health.
By implementing proactive management strategies for calculus teeth, individuals can safeguard their dental health and enjoy a brighter smile for years to come.
An Overview of the Formation of Dental Plaque
Dental plaque is a biofilm that naturally forms on the surface of teeth. It is composed of a combination of bacteria, saliva, and food particles. Plaque begins to form within hours of brushing your teeth, and if left undisturbed, it can harden into tartar, leading to various dental issues. The bacteria in plaque feed on sugars from the food we eat and produce acids that can erode tooth enamel, causing cavities.
One of the key components of dental plaque is Streptococcus mutans, a type of bacteria commonly found in the human mouth. This bacteria is known for its role in the formation of cavities, as it thrives in the acidic environment created by the breakdown of sugars. When plaque is not removed through proper oral hygiene practices such as brushing and flossing, it can build up and eventually mineralize into tartar, which can only be removed by a dental professional.
The formation of dental plaque is a continuous process, and without proper oral care, it can lead to a host of oral health problems. In addition to cavities, plaque buildup can also cause gum inflammation, known as gingivitis, which can progress to periodontitis if left untreated. This highlights the importance of maintaining good oral hygiene habits to prevent the accumulation of plaque and maintain overall oral health.
Common Causes of Tooth Sensitivity
Tooth sensitivity is a common dental problem that can cause discomfort or pain when consuming hot, cold, or sweet foods and beverages. There are several factors that can contribute to tooth sensitivity, including worn tooth enamel, exposed tooth roots, and gum recession. Additionally, cavities, cracked teeth, and gum disease can also lead to sensitivity. Understanding the root cause of tooth sensitivity is essential in addressing the issue effectively.
One common cause of tooth sensitivity is enamel erosion. Enamel is the outermost layer of the tooth that protects the underlying dentin and pulp. When enamel wears down due to factors like acidic foods, aggressive brushing, or teeth grinding, it can expose the dentin, which contains microscopic tubules that lead to the tooth’s nerve center. This exposure to external stimuli can result in sensitivity and discomfort.
Another cause of tooth sensitivity is gum recession, which occurs when the gum tissue pulls back from the tooth, exposing the tooth roots. Since the roots do not have the same protective enamel layer as the crown of the tooth, they are more susceptible to sensitivity. Inadequate oral hygiene practices, periodontal disease, and aging can all contribute to gum recession and subsequent tooth sensitivity. Addressing the underlying cause of gum recession is crucial in alleviating sensitivity and protecting the tooth roots.
The Role of Fluoride in Preventing Tooth Decay
Fluoride is a mineral that plays a crucial role in preventing tooth decay and promoting oral health. It is naturally present in water sources and certain foods, and it can also be found in toothpaste, mouthwash, and professional dental treatments. Fluoride strengthens tooth enamel, making it more resistant to acid attacks from plaque bacteria and sugars in the diet. By remineralizing and repairing early stages of tooth decay, fluoride helps prevent cavities and maintain optimal oral health.
One of the primary ways fluoride protects the teeth is by promoting remineralization, the process of depositing minerals like calcium and phosphate back into the enamel. When the enamel is exposed to acids from plaque bacteria, minerals are lost, making the tooth more vulnerable to decay. Fluoride helps reverse this demineralization process and encourages the remineralization of weakened enamel, strengthening the tooth structure and preventing cavity formation.
In addition to its remineralization properties, fluoride also inhibits the growth of cavity-causing bacteria in the mouth. By reducing the amount of harmful bacteria, fluoride helps maintain a healthy balance in the oral microbiome and decreases the risk of tooth decay. Incorporating fluoride into a daily oral care routine through fluoridated toothpaste and professional fluoride treatments can significantly reduce the likelihood of cavities and support long-term dental health.
**
Conclusion
**
Understanding the formation of dental plaque sheds light on the critical role of oral hygiene in maintaining optimal dental health. Dental plaque, a biofilm composed of bacteria, saliva, and food particles, continuously accumulates on teeth and, if left unaddressed, can solidify into tartar, leading to teeth and gum problems. Streptococcus mutans, a prevalent bacteria in plaque, thrives by metabolizing sugars and producing acids that attack tooth enamel, paving the way for cavity formation.
Tooth sensitivity, a common issue affecting many individuals, can stem from various causes such as enamel erosion and gum recession. Enamel, the protective outer layer of teeth, can wear down due to factors like acidic foods or aggressive brushing, exposing the sensitive dentin underneath. Additionally, gum recession exposes tooth roots lacking enamel protection, making them more susceptible to sensitivity. Addressing these underlying issues and maintaining good oral hygiene practices are paramount in alleviating tooth sensitivity.
Fluoride emerges as a crucial mineral in the prevention of tooth decay and the promotion of oral health. By strengthening tooth enamel and promoting remineralization, fluoride works to combat the detrimental effects of plaque acids and sugars, ultimately reducing the risk of cavities. Furthermore, fluoride inhibits the growth of cavity-causing bacteria, contributing to a balanced oral microbiome and decreased decay potential. Incorporating fluoride through toothpaste and professional treatments significantly bolsters dental health and cavity prevention efforts.